ARTHRITIS

DEFINITION
Arthritis is a disease that affects the joints connecting the bones. It can manifest in both acute and chronic forms and is associated with inflammation of the joints. The patients with arthritis experience pain, stiffness, and discomfort during mobility. Arthritis is swelling and tenderness in one or more joints. Osteoarthritis and rheumatoid arthritis are the most common types of arthritis.
COMMON TYPES OF ARTHRITICS
- OSTEOARTHRITIS (OA)
Osteoarthritis is the most common chronic (long-lasting) joint condition. A joint is the point at which two bones come together. The ends of these bones are protected by cartilage, which is a type of protective tissue. Osteoarthritis causes cartilage — the hard, slippery tissue that covers the ends of bones where they form a joint — to break down, causing the bones in the joint to rub together. Pain, stiffness, and other symptoms may result.
- RHEUMATOID ARTHRITIS (RA)
In rheumatoid arthritis, the body's immune system attacks the lining of the joint capsule, a tough membrane that encloses all the joint parts. This lining (synovial membrane) becomes inflamed and swollen. The disease process can eventually destroy cartilage and bone within the joint.
- GOUT
Gout is a disorder of purine metabolism characterized by hyperuricaemia, deposition of monosodium urate monohydrate crystals in joints and peri-articular tissues and recurrent attacks of acute synovitis. Late changes include cartilage degeneration, renal dysfunction and uric acid urolithiasis. High levels of uric acid in your blood may put you at risk of gout. Gout can be incredibly painful. The most likely affected joint is the one at the base of your big toe, but it can potentially affect other joints as well. You may notice redness, swelling, and excruciating pain in your: toes, feet, ankles, knees, hands or wrists. An acute gout attack can occur within a few hours during the course of a day, but the pain can last for days to weeks. Gout can deteriorate over time.
Acute synovitis (pseudogout) has been linked to the presence of calcium pyrophosphate dihydrate crystals within the affected joint. The patient, typically a middle-aged woman, complains of acute pain and swelling in one of the larger joints – usually the knee. Sometimes the attack is precipitated by a minor illness or operation. The joint is tense and in?amed, though usually not as acutely as in gout.
- ANKYLOSING SPONDYLITIS (AS)
AS is a type of arthritis that mostly affects the spine. It causes severe vertebral inflammation, which can lead to chronic pain and disability. In more severe cases, the inflammation can lead to the formation of new bone on the spine. This may result in deformity. Other parts of your body may experience pain and stiffness as a result of ankylosing spondylitis. Other large joints, such as the shoulders, hips, and knees, can be involved as well.
- JUVENILE ARTHRITIS (JA)
JA is an umbrella term for several types of pediatric arthritis. Juvenile idiopathic arthritis (JIA), formerly known as juvenile rheumatoid arthritis is the most common type. This is a group of autoimmune disorders that can affect the joints of children.JIA first appears in children under the age of 16. It can cause: muscle and soft tissue to tighten, bones to erode, growth patterns to change as well as joints to misalign.
PATHOPHYSIOLOGY
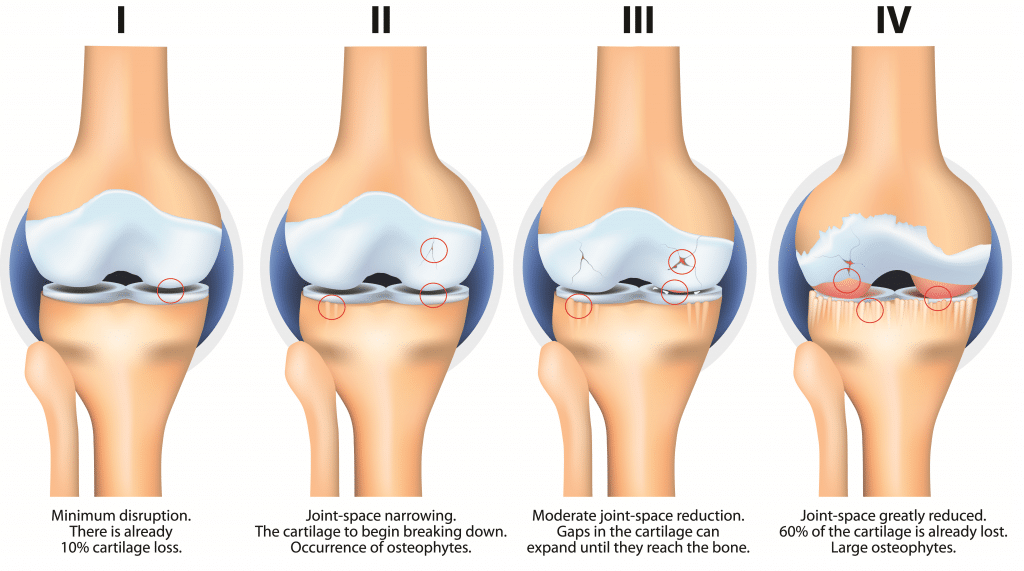
The pathogenesis of Osteoarthritis (OA) involves a degradation of cartilage and remodeling of bone due to an active response of chondrocytes in the articular cartilage and the inflammatory cells in the surrounding tissues. The enzymes released by these cells degrade collagen and proteoglycans, destroying the articular cartilage. Sclerosis occurs as a result of the underlying subchondral bone being exposed, followed by reactive remodeling changes that result in the formation of osteophytes and subchondral bone cysts. Over time, the joint space shrinks progressively. The figure below shows stages of osteoarthritis, as demonstrated in the knee joint
Rheumatoid Arthritis (RA) is an autoimmune disease that is chronic. When the immune system is functioning normally, it recognizes harmful bacteria and viruses and responds by producing an "army" of antibodies that seek out and combat them. In an autoimmune disease, the body incorrectly believes that normal tissues or organs are harmful, resulting in inflammation and damage. In the case of Rheumatoid Arthritis (RA), this effectively results in the body's immune system attacking joint tissues, causing pain and inflammation. RA can cause permanent joint damage, especially in the early stages of the disease. Let's take a closer look at the science behind the onset of RA.
PREDISPOSING FACTORS
- Family history. Some types of arthritis run in families, so you may be more likely to develop arthritis if your parents or siblings have the disorder
- Age
- Your sex
- Previous joint injury
- Post-surgery
- Joint diseases and infection
- Obesity.
RISKS FACTORS
Overweight and Obesity
-
- Infection
- Joint Injuries
- Occupation
- Smoking
- Age
- Gender
- Genetics and Inherited Traits.
TREATMENT
Arthritis treatment focuses on symptom relief and joint function improvement. It is possible that you will need to try several different treatments, or combinations of treatments, before you find what works best for you.
DRUG MANAGEMENT
The medications used to treat arthritis vary depending on the type of arthritis. Commonly used arthritis medications include:
- Painkillers. These medications help reduce pain, but have no effect on inflammation.
- Non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs reduce both pain and inflammation. Over-the-counter NSAIDs include ibuprofen (Advil, Motrin IB, others) and naproxen (Aleve). Some types of NSAIDs are available only by prescription.
- Counterirritants. Some varieties of creams and ointments contain menthol or capsaicin, the ingredient that makes hot peppers spicy. Rubbing these preparations on the skin over your aching joint may interfere with the transmission of pain signals from the joint itself.
Disease-modifying antirheumatic drugs (DMARDs). Often used to treat rheumatoid arthritis, DMARDs slow or stop your immune system from attacking your joints.
Examples include methotrexate (Trexall, Rasuvo, others) and hydroxychloroquine (Plaquenil).
- Biologic response modifiers. Typically used in conjunction with DMARDs, biologic response modifiers are genetically engineered drugs that target various protein molecules that are involved in the immune response. Biologic response modifiers come in a variety of forms. TNF (tumor necrosis factor) inhibitors are frequently prescribed. Etanercept (Enbrel, Erelzi, Eticovo) and infliximab are two examples (Remicade, Inflectra, others).
- Corticosteroids. Prednisone (Prednisone Intensol, Rayos) and cortisol (Cortef) are examples of drugs in this class that reduce inflammation and suppress the immune system. Corticosteroids can be ingested or injected directly into the painful joint.
PHYSIOTHERAPY TREATMENT
Physical therapy can be helpful for some types of arthritis. Exercises can improve range of motion and strengthen the muscles surrounding joints. In some cases, splints or braces may be warranted.
The Goals of Physical Therapy For arthritis typically include:
- Improving the mobility and restoring the use of affected joints,
- Increasing strength to support the joints,
- Maintaining fitness,
- Preserving the ability to perform daily activities.?
To begin, an individualized exercise plan is created. These exercises are intended to improve flexibility, strength, coordination, and balance in order to achieve peak physical performance. Physical therapist:
- Show you how to use assistive devices like walkers and canes properly.
- To relieve pain and improve function, teach you proper posture and body mechanics for common daily activities.
- Recommend various treatment options, such as braces and splints to support joints, shoe inserts to relieve stress on the lower extremities, and hot and cold therapy to relieve joint pain and inflammation.
- Suggest modifications to your environment, such as ergonomic chairs or a cushioned mat in your kitchen, to relieve pain and improve function.
Role of Physiotherapy in treating Osteoarthritis
Osteoarthritis mainly affects knee joints, hips, spine, and fingers. PT is recommended in patients suffering from osteoarthritis because it benefits the patients by improving physical functioning and reducing pain. Several modalities used by physiotherapists for treating osteoarthritis include: Exercises, Massages, Providing patients with walking aids and Electrotherapy.
Role of Physiotherapy in treating Rheumatoid Arthritis (RA)
Before beginning treatment, physiotherapists usually conduct a physical assessment test. The gait, daily life activities, range of joint motion, muscle strength test, posture, and respiratory function are all evaluated. Following that, they use the arthritis impact measurement scale and the health assessment questionnaire to make a more precise assessment.
DIETS
- Fatty Fish. Fatty fish varieties such as salmon, mackerel, sardines and trout are high in omega-3 fatty acids, which have been shown to have potent anti-inflammatory effects
- Garlic.
- Ginger
- Broccoli
- Walnuts
- Berries
- Spinach
- Grapes.
Protecting your health information at every step.
Who we are
Tibabu is your go to health and medical centre, we combine our passion for love with our love for humanity. We understand that your health defines us and believe that we are God's instruments, dedicated to delivery of the best quality healthcare.
Useful Links
Our Contacts
Dereshe Towers Off Murang'a Road,
Ngara, 4107 - 00506, Nairobi